Last year, on a walk in the city, my boyfriend and I witnessed a young woman in her 20s fall from her chair onto the floor. She was out to dinner with her partner. We heard him cry out because she was not responding. My boyfriend is a physician completing his surgical residency, and I am a critical care registered nurse, so we ran over to help. She was not breathing, and I did not feel a pulse.
We started cardiopulmonary resuscitation (CPR) while the restaurant server called 911. My boyfriend and I used to live in New York City, and remembered signs saying “Automated external defibrillator (AED) behind the bar.” We asked for one, but the restaurant didn’t have one. We asked any person who stopped to help to look for a defibrillator from any nearby store, restaurant, or building.
Each of them ran desperately in opposite directions. We continued CPR while waiting for the emergency medical services to arrive. People returned one by one saying that they could not find an AED.
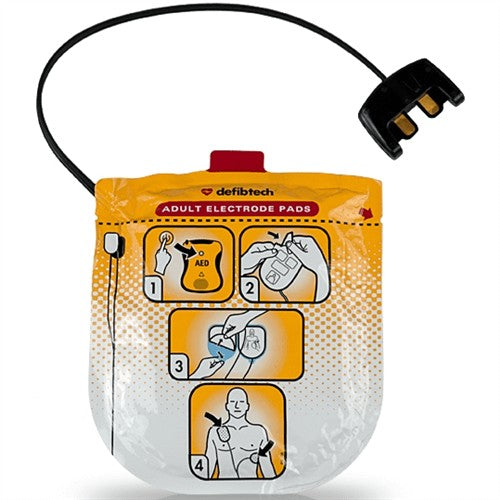
Approximately 15 minutes passed. The EMS finally arrived and took over CPR. They placed the pads from the defibrillator onto the young woman, and the electrodes delivered a shock. She regained a pulse but still did not wake up. The EMS worked to keep her alive, and we were left consoling her partner. They kept trying, then brought her to the hospital. I don’t know if she survived.
“I don’t know if she survived.”
When the heart stops, within three minutes, the brain and organs are no longer getting the blood and oxygen they need. By nine minutes, irreversible brain damage has likely occurred. It took 15 minutes for EMS to arrive, during which time we were hunting for a small, relatively inexpensive device that could have saved this young woman’s life.
During that time, we were providing CPR, but that only restores partial blood flow to the heart and brain, even when delivered by trained providers. Experts say that in about half of deaths from cardiac arrests, the person suffers from an irregular heartbeat called ventricular fibrillation. If that happens, an AED can restore the heart to a regular rhythm.
AEDs are very effective. According to the American Heart Association, nine in 10 cardiac arrest victims who receive a shock from an AED within the first minute survive. This makes AEDs essential for saving lives outside the hospital.
Some cities like New York have made access to AEDs a priority; in that city, schools, public buildings, and any facility where at least 75 people gather (such as a bar or restaurant) are required to have an AED on-site, and train at least one employee how to use it. This is not the case in Pennsylvania, New Jersey, and many other states.
AEDs were designed to be simple, so anyone could use them in an emergency. They typically cost less than $2,000 — and if they save one person’s life, that’s a bargain. I cannot understand how AEDs can be in nearly every public space in a city like NYC, but nowhere to be found in another large city: Philadelphia.
This is a major public health concern. More than 350,000 Americans experience heart attacks outside the hospital every year, and 90% of those people die.
There is no easy solution to this problem, but a critical first step is to make AEDs publicly available and more easily accessible. They do not require a prescription, are lightweight, and are portable. We need to raise awareness of their importance so they are stocked in public areas.
More than one year later, I still think about the young woman my boyfriend and I couldn’t save, and what might have happened if we’d had an AED.
is pursuing a doctorate in nursing anesthesia at the University of Pennsylvania.
Published
July 19, 2022